Disc Bulge
Physiotherapy for Disc Bulges & Disc Degeneration
Targeted Treatment to Reduce Pain, Improve Movement & Restore Spine Health
Disc bulges and disc degeneration (degenerative disc disease) are common causes of lower back and neck pain. These conditions can create irritation around joints, nerves and surrounding soft tissues, leading to stiffness, muscle spasm, sciatica and reduced daily function. Our physiotherapists provide evidence-based assessment and personalised treatment plans to relieve pain, restore mobility and strengthen the spine for long-term resilience.
Understanding Disc Bulges & Disc Degeneration
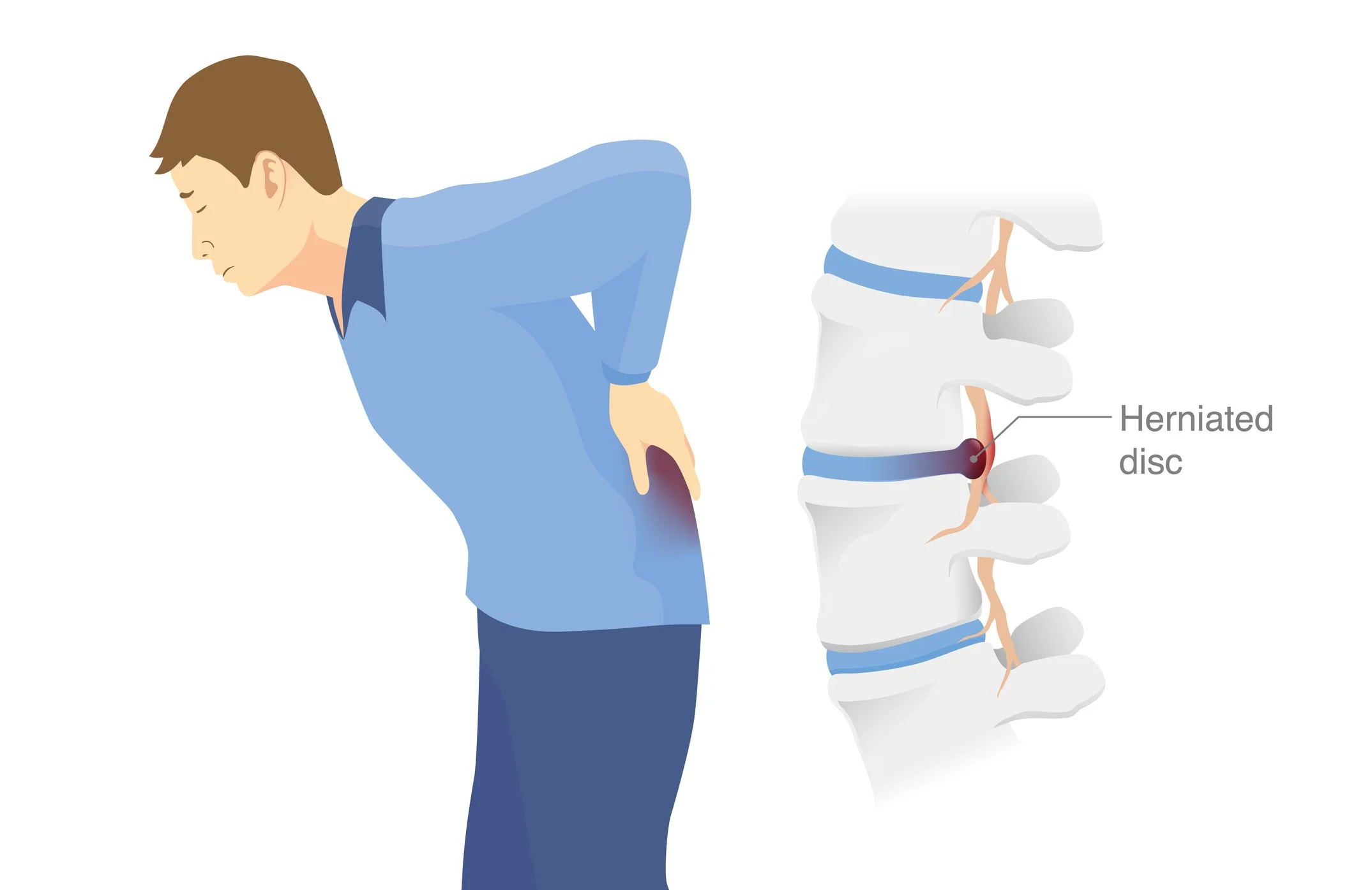
A disc bulge occurs when the disc material protrudes outward, potentially irritating nearby structures such as the nerve roots.
Disc degeneration involves age-related or load-related changes in the discs, including reduced hydration, height loss and stiffness.
Common symptoms include:
Localised back or neck pain
Sciatica or radiating leg/arm pain
Tingling or numbness
Central or unilateral stiffness
Pain with bending, sitting or lifting
Reduced mobility or strength
With the right guidance, most disc-related conditions improve significantly through physiotherapy.
Disc Bulge
A disc bulge happens when the disc’s outer ring weakens and the inner gel pushes outward, usually evenly around the disc rather than in one direction. It commonly affects the lower back and neck, can narrow the space for nerves, and causes local pain or stiffness. If nerves are squeezed it can cause numbness, tingling or weakness that radiates. Causes include ageing, repeated loading, poor posture and sudden strain. Diagnosis is by exam, with imaging if needed. Treatment is usually non-surgical: pain relief, hands-on therapy, specific exercises to restore movement and load tolerance, and advice on activity; surgery is for ongoing or worsening nerve problems.
Areas We Treat for Disc Bulges & Disc Degeneration
1. Pain & Inflammation Management
Techniques to reduce pain and muscle spasm
Gentle movement strategies to calm irritation
Positioning advice for sitting, sleeping and lifting
Modalities as needed (heat, gentle traction, soft tissue work)
2. Restoring Spine Mobility & Flexibility
Loss of movement is a major contributor to disc pain. We use:
Lumbar and cervical joint mobilisation
Gentle extension or flexion-based exercises depending on your pattern
Nerve mobility techniques for sciatica
Soft tissue treatment to reduce guarding
3. Core Stability & Lumbar/ Cervical Strengthening
Targeted strengthening is essential for long-term recovery. Programs include:
Core strengthening exercises
Glute and hip stabiliser strengthening
Thoracic mobility and postural strengthening
Progressive strengthening for lifting and daily activity
4. Functional Movement & Posture Training
Correcting load and movement patterns helps prevent flare-ups. We focus on:
Hip hinge mechanics to reduce disc pressure
Safe bending, lifting and daily movement strategies
Postural endurance training for work and home
Ergonomic guidance for sitting and standing
5. Nerve Pain & Sciatica Management
For patients with nerve referral, treatment may include:
Sciatic or cervical nerve gliding
Reducing neural tension
Re-conditioning of affected muscles
Load progression tailored to nerve irritability
6. Graded Activity & Return-to-Function Programs
To help you return confidently to your lifestyle, we offer:
Work-specific strengthening
Return-to-sport conditioning
Walking and gym progression programs
Endurance building for spinal stability
7. Chronic & Recurrent Disc Pain Management
For long-standing issues, we provide:
Detailed biomechanical assessment
Long-term strength and mobility programs
Education on flare-up prevention
Strategies for disc health and load control
Our Physiotherapy Approach
Your treatment is tailored to your symptoms, imaging (if applicable) and functional goals. Our approach includes:
Manual therapy
Individualised exercise prescription
Spinal mobility restoration
Lumbar and cervical stability training
Postural and ergonomic education
Return-to-activity planning
Flare-up management advice
Our aim is to help you rebuild strength, restore confidence and move freely without fear.
Common Causes & Contributing Factors We Treat
Poor lifting or bending mechanics
Prolonged sitting or poor desk posture
Weak core or gluteal muscles
Age-related changes in the discs
Repeated flexion or rotation strain
Sudden heavy lifting
Deconditioning or inactivity
When to Seek Physiotherapy
Book an assessment if you experience:
Persistent or worsening back/neck pain
Sciatic leg pain or nerve symptoms
Difficulty sitting, bending or lifting
Recurrent flare-ups
Stiffness that limits daily function
Pain lasting more than a few days
Early intervention leads to faster improvement and reduced recurrence.
Book Your Disc Pain Assessment
If you’re dealing with disc bulges, disc degeneration or recurring back/neck pain, our physiotherapists can help you recover safely and confidently.
Contact us today to book your appointment.